- Physiological Jaundice is very common with almost all neonates affected
- This is jaundice arising after 24 hours and resolving with 14 days (21 in premature infants)
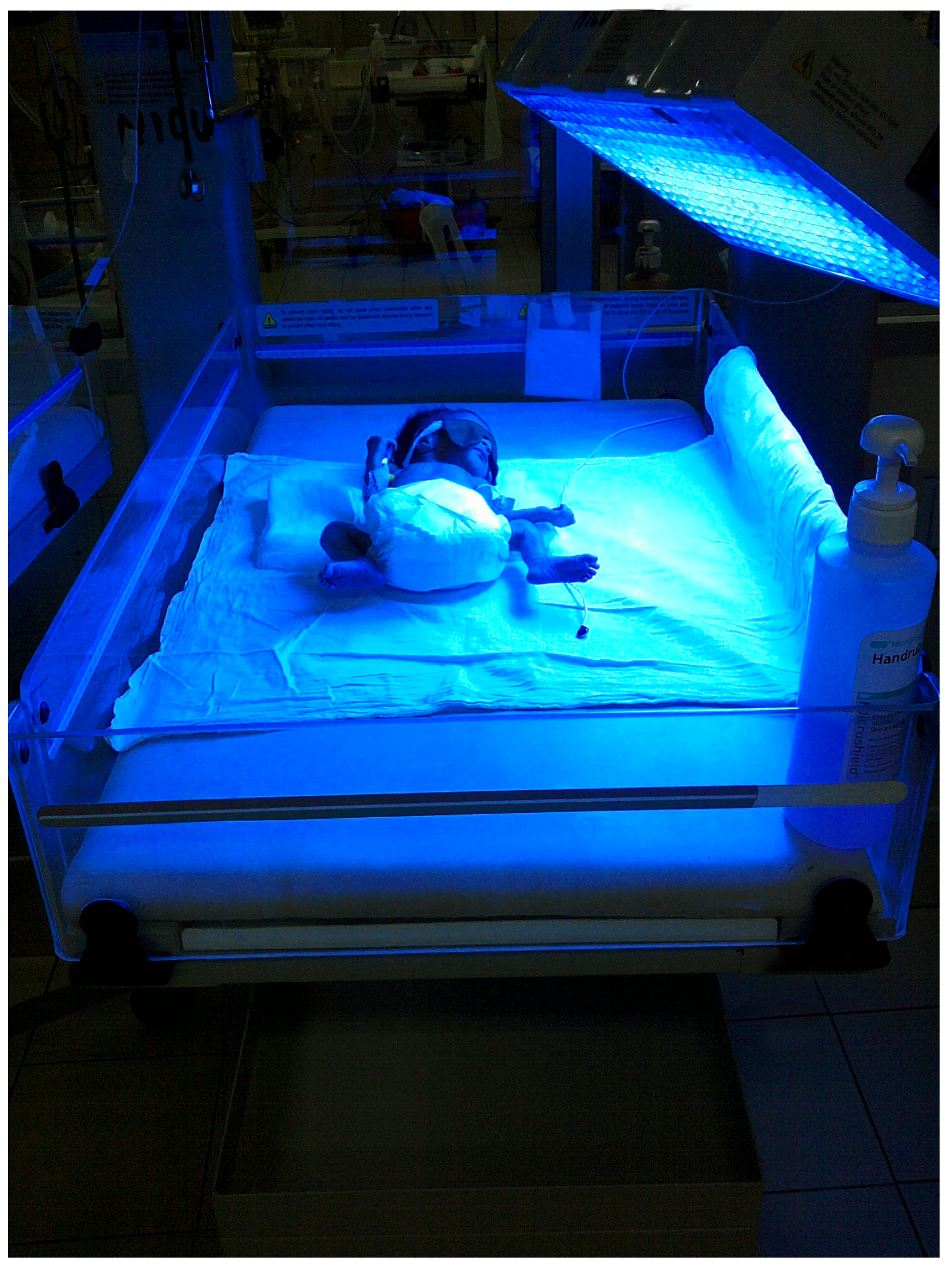
- It may require treatment with phototherapy
- Jaundice may be more severe in: preterm infants, sepsis, severe heamolysis (due to Rh-incompatibility, ABO incompatability, G6PD deficiency, spherocytosis) and bruising (cephalohaematoma or subgaleal haemorrhage)</li>
- In a child felt to be clinically jaundiced, the level should be checked and plotted on a gestationally appropriate chart (NICE Guideline on Jaundice)
Press PLAY to start supplementary narration
