A diagnosis of Inflammatory Bowel Disease (IBD) is likely for Alfie with these results; although 25% of patients with new IBD can have normal inflammatory markers at presentation.
Crohn's Disease (CD) and Ulcerative Colitis (UC) are the two main forms of Inflammatory Bowel Disease; 10% of cases are Indeterminate Colitis (IC), with an absence of features specific enough to identify UC or Crohn’s.
IBD in children has an incidence of 12 per 100 000 under 16 years of age, with an 80% increase in incidence in the past 10 years, and 25% of all new IBD patients present before 18years of age. The lifetime risk of Crohn’s rises to 5-10% in those with a first degree relative with IBD. . It is slightly more common in boys and there is a slightly higher rate of UC in Asian children than in other ethnic groups.
The mean age at diagnosis is 11.9 years, with many teenagers presenting during their pubertal growth spurt. Crohn’s disease is twice as common as ulcerative colitis. The precise aetiology of IBD is multifactorial but recent evidence suggests that IBD is caused by a combination of factors: genetic predisposition, immune dysfunction, diet, host bacteria and environmental triggers (viral infection, stress, and drugs).
Based on a study of 40,000 children in Norwich, there is an increased background risk of IBD in those who eat more fatty, fast foods, and a lower risk in those who eat a Mediterranean diet rich in omega3 fatty acids (e.g. olive oil/fish)
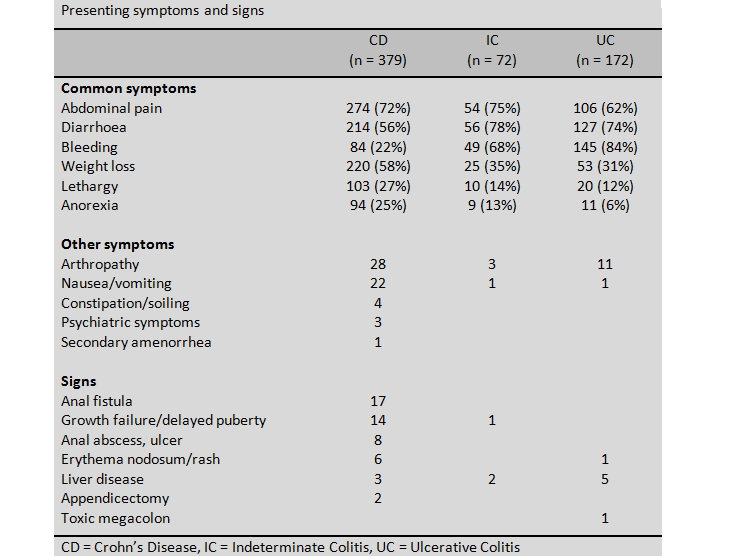
The most common symptoms of IBD in children are abdominal pain, diarrhoea, bleeding, weight loss, lethargy and anorexia. The table above illustrates which features are most likely to be present at diagnosis in patients with Crohn's (CD), Ulcerative Colitis (UC) or Indeterminate Colitis (IC).